Ethical fears of organ harvesting during “brain death”
Many who obtain a driver’s license elect to become organ donors. In general, organ donation is perceived as an altruistic act without ethical controversy.
The Catechism of the Catholic Church states, “Organ donation after death is a noble and meritorious act and is to be encouraged as an expression of generous solidarity” (emphasis added; CCC 2296). The presupposition is that donation of critical organs occurs only after the person is dead.
However, there is controversy regarding whether a person declared “brain dead” is, in fact, dead.
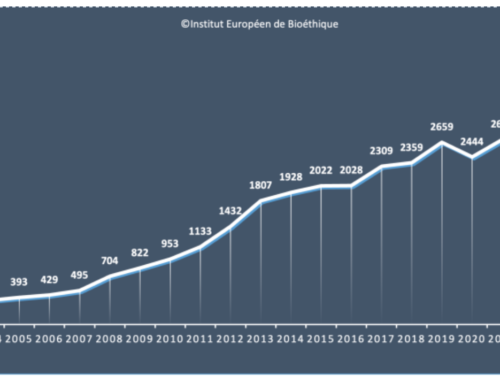
Organ donation typically occurs in the following context: a young, formerly completely healthy person has a sudden severe brain injury (SBI). Within two days, the person is declared “brain dead” and his or her organs are harvested.
We know that when a computer crashes, it initially boots up into safe mode. Safe mode has reduced functionality. Once the operating system is repaired in safe mode, the computer can return to full function.
Similarly, when the brain is injured, it may initially enter a “safe mode” during which functionality is substantially decreased, but brain viability is preserved. This condition is called global ischemic penumbra (GIP) and can last up to two days. It is important to note that during the period of GIP a person will meet all the criteria for brain death as defined by the American Association of Neurology
Note the time frame: organ donation typically occurs within two days after injury, which is precisely how long GIP lasts.
Therefore, it seems at least possible that a “brain dead” person’s organs could be harvested prior to that person actually being dead. There are many stories of young people declared “brain dead” whose families refused organ harvesting and who subsequently experienced complete or near-complete recovery. It is impossible to know how many of those declared “brain dead” whose organs were harvested may also have recovered if given sufficient time and appropriate medical care.
The notion of brain death has critical implications for the entire pro-life movement because it seems to endorse a performance theory of personhood. In this framework, a human has rights if he or she can behave like a person; specifically, if one can demonstrate intellect and will. “Marginal” humans (such as the unborn) are denied rights because they cannot demonstrate intellect and will.
In contrast, we as Catholics embrace an endowment theory of personhood. Personhood is not grounded in how we act, but in the type of being we are. When a child displays intellect and will for the first time, he or she does not instantly “become” a person. Rather, that personhood was always present because he or she always possessed the intrinsic capacity for rationality even if it was not displayed.
Humans with SBI in a state of GIP are not nonpersons but rather wounded persons. If we harvest the organs of such humans because they cannot display intellect and will, we set a dangerous precedent by seemingly affirming a performance theory of personhood. Are we acting hypocritically if we defend the life of the unborn but not the life of those with SBI?
This brief article cannot fully address the complex topic of brain death. Rather, the purpose of this article is to raise awareness of the ethical concerns regarding critical organ donation, which is predicated on the validity of the notion of brain death. Further study is highly encouraged not simply for ourselves, but also for the young people in our lives — such as a child or grandchild about to get a driver’s license and make the critical decision: should I be an organ donor?
DR. JOSEPH M. EBLE is a radiologist practicing in Tulsa, OK. He is president of the Tulsa Guild of the Catholic Medical Association and a member of the Tulsa Chapter of Legatus.